|
VIETNAMESE GERMAN SCIENTIFIC SYMPOSIUM 2017 Nha Trang/Khanh Hoa 28.11.2017 20 Years Anniversary of the German Vietnamese Association of Cardiology (DVFK) Venue: KHANH HOA HOSPITAL Time: 13:30 – 17:00 Organization: . Vietnamese Heart Association Khanh Hoa . Khanh Hoa Hospital . German Vietnamese Association of Cardiology/ Deutsch-Vietnamesischer Förderkreis für Kardiologie e.V. (DVFK) . Vietnamese German Academy for Science and Education in Cardiology and Cardiovascular Surgery (VGAC) . Vietnamese German Faculty of Medicine of Pham Ngoc Thach University of Medicine at Ho Chi Minh City (VGFM) Lectures: Echocardiography in oncological diseases Dr. Irmtraut Kruck, Cardiology Clinic, Ludwigsburg, Germany Echocardiography for early detection of cardio toxicity in cancer-patients chemotherapy induces impairment of LV- and RV structure, function and mechanics by different complex mechanism. For this comprehensive assessment of LV/RV structure function and mechanics is necessary in cancer patients before, during and after treatment. Echocardiography is the best image modality because of its availability in every day clinical practice and allows early detection of reduced LV- and RV-function. Therefore it is necessary to perform an echocardiographic examination including all available technics (pulsed and tissue Doppler and 2-D-Strain) in echocardiographic laboratories which have the appropriate equipment and diagnostic expertise. Cardiac dysfunction caused by cardiotoxic treatment can appear at any time during or after therapy and sometimes even after years. Recommendations on the frequency of standardized follow-up examinations exist, but they vary between the specialist societies. Increased morbidity and mortality due to cardiotoxic treatment are now well known, but still too few patients undergo appropriate examinations. Early detection and treatment of existing heart failure and treatment should improve the clinical outcome of these patients. Beyond coronary angiography: Why do we need additional invasive techniques? Prof.Dr. Volker Klauss, Cardiology Munich City Centre, Munich, Germany The decision for interventional treatment of a coronary lesion should be based on symptoms and prove of ischemia. However, in clinical practice, stenoses are often treated depending on the angiographic image, because symptoms are not clear and tests for ischemia have not been performed or the tests are inconclusive. By means of intracoronary pressure measurements (i.e. determination of fractional flow reserve – FFR, or instantaneous wave-free ratio - iFR) the hemodynamic relevance of a coronary stenoses can be determined during coronary angiography especially in intermediate lesions and thus the decision to treat or not to treat is based on an objective test of ischemia. Regarding coronary morphology angiography is the standard for imaging of the coronary tree. However, this technique has limitations. Intravascular ultrasound (IVUS) allows a cross-sectional view of the coronary arteries. IVUS may help to diagnose and assess stent underexpansion and malapposition and to guide interventions in complex cases. Another recent modality based on infrared light is the optical coherence tomography (OCT)with a resolution better than IVUS. It is now used for evaluation of new stent technologies i.e. bioabsorbable scaffolds. Transcatheter treatment of severe mitral regurgitation using the mitraclip system Prof. Dr. Florian Krötz, Clinic Starnberg, Department of Cardiology, 82319 Starnberg, Germany The interventional treatment of mitral valve regurgitation using the MitraClip procedure is a valuable tool for treatment of inoperable patients or patients at high operative risk. Its efficiency in reducing mitral regurgitation has been proven in the EVEREST II study, and use of the technique has rapidly grown worldwide and especially in Germany since then. In suitable patients the method is excellent for treating primary mitral valve regurgitation but has also great potential in patients with heart failure and secondary mitral valve regurgitation, which often show poor outcomes following surgery. Current recommendations and clinical data concerning the method rely largely on data from the EVEREST II trial. Registries, like the German TRAMI register however, survey a large number of patients, so today there is a good insight into the prerequisites of building an interventional mitral valve program, the need for specialized screening of patients, and for a dedicated interventional setup during implantation. This and the essential procedural techniques will be outlined. Catheter Ablation of Atrial Fibrillation in Patients with heart Failure: Evidence for prognostic indication? Dr. Dinh Quang Nguyen, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Catheter Ablation of Atrial fibrillation is well established in symptomatic patients. But it is still a symptomatic indication. In Patients with reduced LV ejection fraction and heart failure, the success rate of catheter ablation remains challenging and controversial. This presentation gives an update in publications and highlights a new published randomized study (Castle-AF), which has shown a prognostic benefit of catheter ablation in Patients with heart failure. Diagnosis and Management of patients with inherited primary arrhythmia syndromes Risk stratification in a family with Long QT-Syndrome Dr. Birgit Gerecke, outpatient center cardiology Peine When the diagnosis of an inherited primary arrhythmia syndrome is made, considerations on the management also of other family members are required. This is shown exemplary in a family with LQTS. A 16 year old girl presented with recurrent syncope. The examinations of the family doctor contained an ECG. A prolongation of the QT interval was seen without a secondary cause of QT prolongation. The patient was admitted to a hospital. ECG monitoring showed runs of torsades de pointes VT. Beta blocker therapy was initiated, but still runs of VT were present. The diagnosis of a LQTS 2 was established. Family history revealed a sudden cardiac death in a great uncle of the index patient. ICD implantation was discussed and after informed consenta single chamber ICD system was implanted. Till now there has been no adequate shock delivery in the patient. ECGs of the parents and two siblings were done. The mother also presented with a QT prolongation, but till now is asymptomatic. A younger sister has a borderline QTc, the ECG of the brother showed a normal QTc. Genetic testing was done in the family with the presence of an LQTS gene mutation (KCNH2mutation) in the index patient. This mutation was also found in her mother, but not in the siblings. LQT-Syndrom is an inherited arrhythmia syndrome with a broad spectrum of clinical presentations, even in one family. A family based genetic testing can help to stratify the management. An exclusion of an assured mutation of the index patient in other family members can rule out the risk of a rhythmogenic disease and event with a high probability. Life style changes are recommended for family members with the mutation containing the avoidance of QT prolonging drugs, the identification and correction of electrolyte abnormalities, beta-blockers or ICD-implantation depending on the clinical presentation. Approximately 20-25 % of patients with LQTS confirmed by the presence of an LQTS gene mutation may have a normal QTc. Provocative tests with QT measurement e.g. in the recovery phase of exercise testing can help to unmask these patients. Diagnostic value of cardiac MRI in patients with heart failure Dr. Birke Schneider, Lübeck, Germany Heart Failure (HF) is a clinical syndrome characterized by typical symptoms and clinical signs which are caused by a structural and/ or functional cardiac abnormality, resulting in reduced cardiac output and/ or elevated intracardiac pressures at rest or during stress. Demonstration of an underlying cardiac cause is central to the diagnosis of HF. This is usually a myocardial abnormality causing systolic and/or diastolic ventricular dysfunction. However, abnormalities of the valves, pericardium, endocardium, heart rhythm and conduction can also cause HF, and more than one abnormality is often present. Identification of the underlying cardiac problem is crucial for therapeutic reasons, as the precise pathology determines the specific treatment used. Cardiac imaging plays a central role in the diagnosis of HF and in guiding treatment. Of several imaging modalities available, echocardiography is the method of choice in patients with suspected HF, for reasons of accuracy, availability (including portability), safety and cost. However, the reliability of the echocardiographic study is highly dependent on the operator and centre experience and the image quality. Transthoracic echocardiography (TTE) nevertheless is regarded the primary method for assessment of systolic and diastolic function of both left and right ventricles and for the evaluation of valvular function. Cardiac magnetic resonance imaging (CMRI) is nowadays acknowledged as the gold standard for the measurements of volumes, mass and ejection fraction of both the left and right ventricles (Class I Level C in the ESC Guidelines on HF 2016). It is the best alternative cardiac imaging modality for patients with nondiagnostic echocardiographic studies (particularly for imaging of the right heart) and is the method of choice in patients with complex congenital heart diseases. In addition, CMRI also allows tissue characterization and thereby can be useful for establishing HF aetiology. CMRI is the preferred imaging method to assess myocardial fibrosis using late gadolinium enhancement (LGE) along with T1 mapping. CMRI with LGE allows differentiation between ischaemic and non-ischaemic origins of HF and myocardial fibrosis/ scars can be visualized. Different hyperenhancement patterns result from the pathophysiology of the underlying disease and help to establish the correct diagnosis. CMRI may also be used for the assessment of myocardial ischaemia and viability in patients with HF and coronary artery disease. Various patients are presented where CMRI was essential in finding the cause of HF and had implications for patient management. Clinical limitations of CMRI will also be discussed. Risk of major adverse cardiac events following noncardiac surgery in patients with coronary stents Prof. Dr. Hans-F. Voehringer, DRK Clinics Berlin, Germany Surgeons, cardiologists, primary care physicians, and anesthesiologists frequently have to determine the antiplatelet management in patients with coronary heart disease undergoing elective surgery. In Germany, more than 300 000 patients receive coronary stents annually, with up to 20% of these individuals requiring non-cardiac surgery within 2 years. There is definitive evidence that patients who have undergone percutaneous coronary interventions with stent implantation are at increased risk of perioperative major cardiac events (MACE) and that the risk is moderated by stent type (bare metal stent [BMS] vs. drug eluting stent [DES]), operative urgency, early discontinuation of antiplatelet therapy, and time from coronary intervention. Guidelines recommend delaying non-cardiac surgery in patients after coronary stent procedure for 1 year after DES and for 6 weeks after BMS. The evidence underlying these recommendations is limited and conflicting. In a systematic review the perioperative antiplatelet management will be assessed to help clinicians with this common clinical case. A comprehensive investigation of systolic and diastolic heart failure patients by echocardiography PD Dr. Wolfgang Fehske, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Left atrial function, what can we derive from echocardiographic examinations with special respect to prognosis of stability after electrophysiological ablation for atrial fibrillation Mareike Juliana Brunold, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Sudden cardiac death beyond the existing guidelines: Does the Life Vest concept opens better solutions for our patients? Stefan Winter, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany FACULTY: Dr. Mareike Juliana Brunold, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany PD Dr. Wolfgang Fehske, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Dr. Birgit Gerecke, outpatient center cardiology Peine, Germany Prof. Dr. Volker Klauss, Cardiology Munich City Centre, Munich, Germany Prof. Dr. Florian Krötz, Clinic Starnberg, Department of Cardiology, 82319 Starnberg, Germany Dr. Irmtraut Kruck, Cardiology Clinic Ludwigsburg, Germany Dr. Dinh Quang Nguyen, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Prof. Dr. Si Huyen Nguyen, Vietnamese German Faculty of Medicine at Pham Ngoc Thach University HCMC, HELIOS St. Marienberg Hospital Helmstedt, Germany Dr. Birke Schneider, MD, Lübeck, Germany Prof. Dr. Hans-F. Voehringer, DRK Clinics Berlin, Germany Stefan Winter, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Visite auf einer Station der kardiologischen Abteilung v.l. S. Klauss (München), Dr. I. Kruck (Ludwigsburg), Dr. B. Gerecke (Peine), Dr. M.J. Brunold (Köln), Dr. B. Schneider (Lübeck)
0 Comments
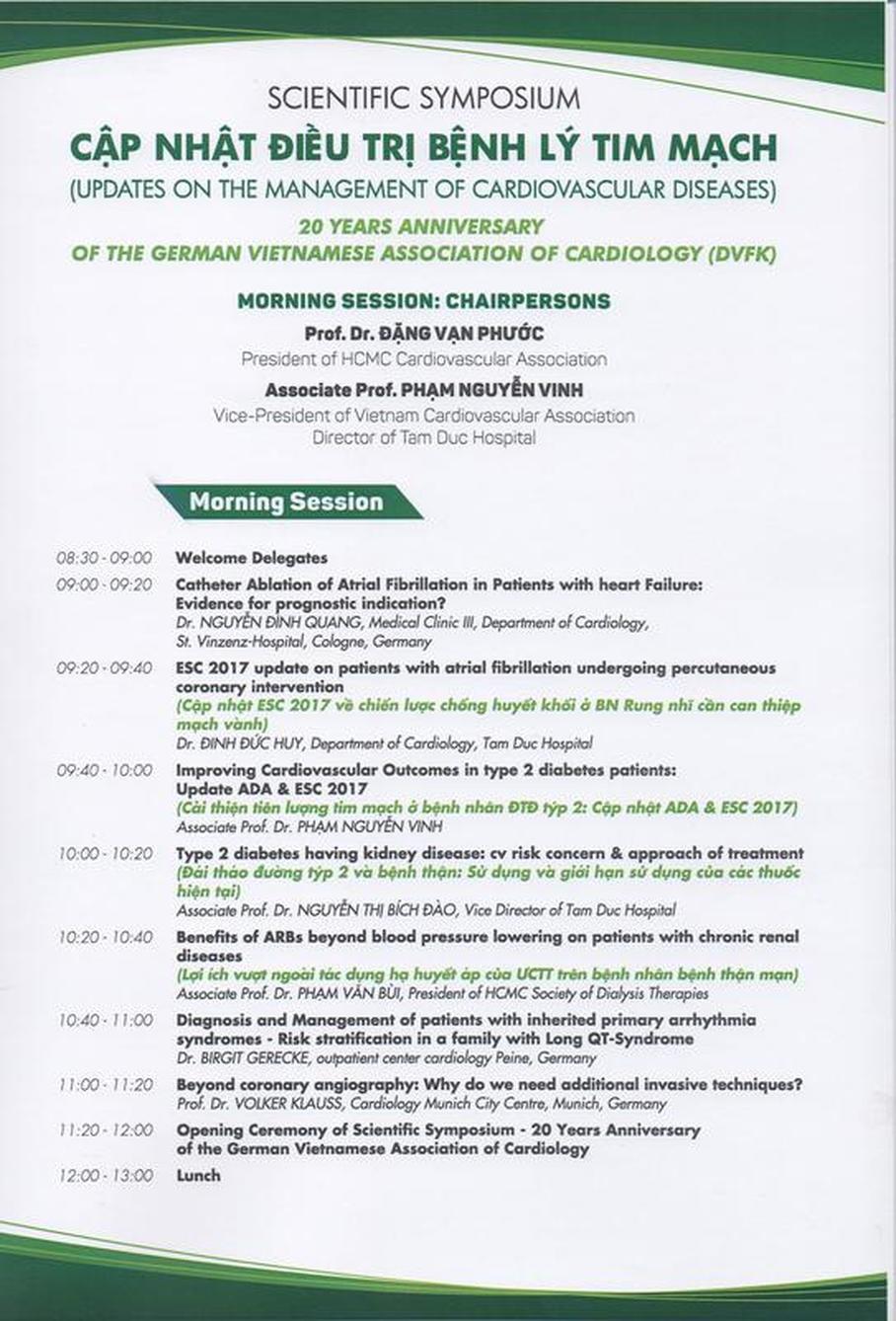
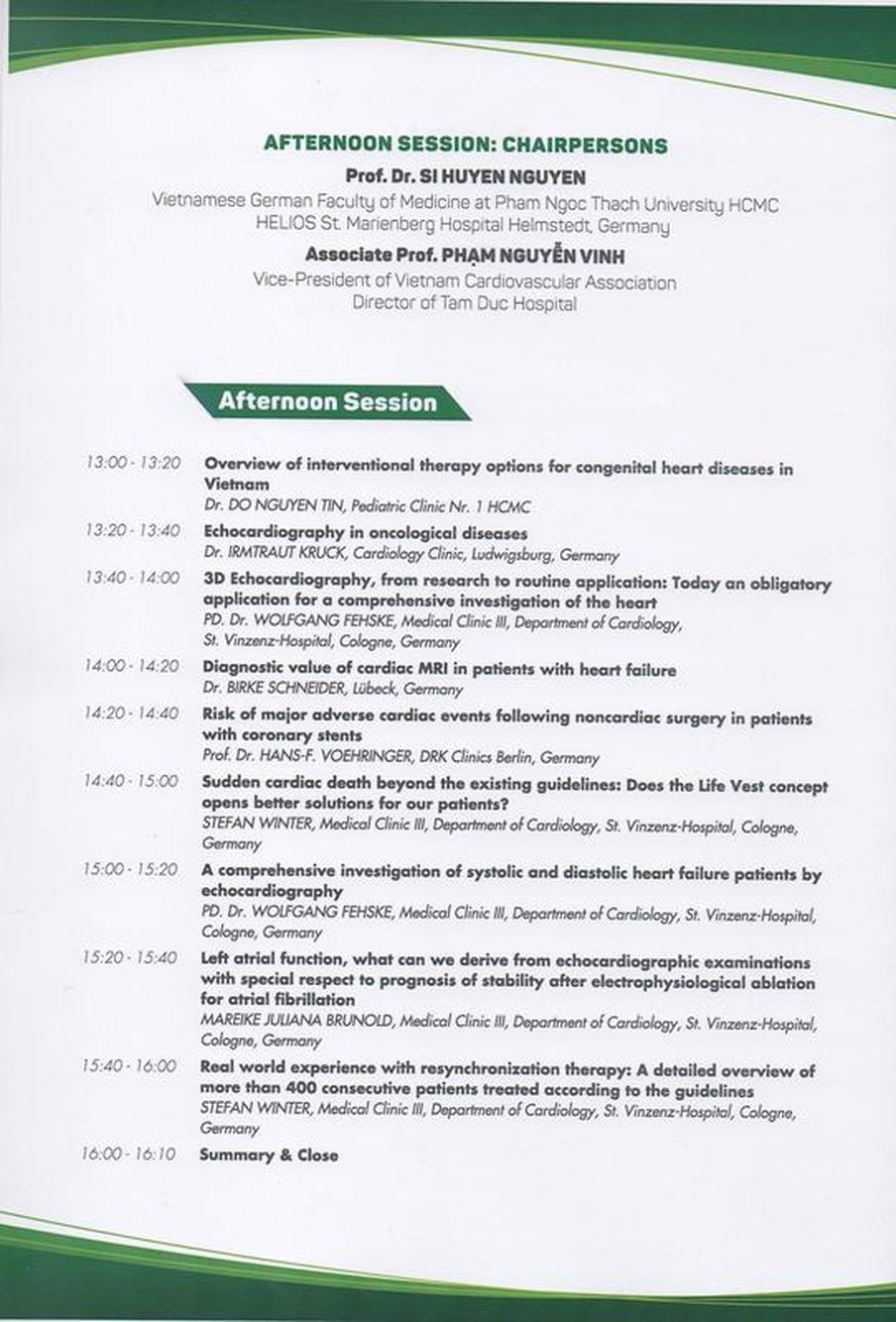
17. VIETNAMESE GERMAN HEART DAYS HCMC 26.11.2017 Venue: NEW WORLD HOTEL, 76 Le Lai Street, District 1, HCMC Time: 08:30 - 16:30 Organization: HCMC Cardiovascular Association in Cooperation with
 v.l. Dr. B. Schneider (Lübeck), S. Klauss (München), Dr. B. Gerecke (Peine), Prof. PV Bui (HCMC), Prof. H.-F. Vöhringer (Berlin), Prof. V. Klauss (München), Prof. NT Binh (HCMC), Prof. SH Nguyen (HCMC/Helmstedt), Dr. G. Haug (Bayerisch Gmain), Prof. DV Phuoc (HCMC), Prof. PN Vinh (HCMC), Dr. S. Winter (Köln), PD Dr. W. Fehske (Köln), Dr. I. Kruck (Ludwigsburg), Dr. DQ Nguyen (Köln), Dr. MJ Brunold (Köln) |
Archiv
November 2019
|









 RSS Feed
RSS Feed
