|
FACULTY:
Prof. Dr. Wolfgang Fehske, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Dr. Claus Fleischmann, Medical Clinic I, Department of Cardiology, Clinic Wolfsburg, Germany Dr. Birgit Gerecke, Heart Center at the University Medical Center Göttingen, Germany Dr. Christian Glatthor, Cardiovascular Center Bodensee-Oberschwaben, Ravensburg- Weingarten, Germany Prof. Dr. Volker Klauss, Cardiology Munich City Centre, Munich, Germany Prof. Dr. Florian Krötz, Clinic Starnberg, Department of Cardiology, 82319 Starnberg, Germany Prof. Dr. Bernd Lemke, Department of Cardiology, Electrophysiology and Angiology, Klinikum Lüdenscheid, Germany Dr. Dinh Quang Nguyen, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Prof. Dr. Si Huyen Nguyen, Vietnamese German Faculty of Medicine at Pham Ngoc Thach University HCMC, HELIOS St. Marienberg Hospital Helmstedt, Germany Dr. Klaus Schlotterbeck, FESC, MBA, Cardiovascular Center Bodensee-Oberschwaben, Ravensburg-Weingarten, Germany Dr. Benno Schwartz, Cardiologist, 38350 Helmstedt Prof. Dr. med. Vanadin Regina Seifert-Klauss, Interdisciplinary Endometriosis Center, University Hospital rechts der Isar, Munich, Germany Prof. Dr. Hans-F. Voehringer, DRK Kliniken Berlin, Germany PD Dr. Werner Zwehl, Cardiologist, 0638 München, Germany
0 Comments
Datum: 07.09.2019 Ort: Ärztehaus, An der Petrikirche 1, 38100 Braunschweig Sehr geehrte Frau Kollegin, sehr geehrter Herr Kollege, wir möchten Sie gern auch dieses Jahr wieder zu unserer Jahrestagung herzlich einladen. Für 2019 haben wir drei interessante Sitzungen für Sie zusammengestellt; für die I. Sitzung haben wir das Thema Klappenerkrankungen ausgewählt, die II. und III. Sitzung widmen sich Themen, die für den klinischen Alltag wichtig sind. Unsere 23. wissenschaftliche Jahrestagung mit den Themen: AKTUELLE KARDIOLOGIE & INTERESSANTE KASUISTIKEN findet in diesem Jahr wie gewohnt in Braunschweig zusammen mit eingeladenen Gästen aus Vietnam in Zusammenarbeit mit der Ärztekammer Niedersachsen Bezirksstelle Braunschweig und dem Ärzteverein Braunschweig statt. Wir möchten Sie hiermit herzlich nach Braunschweig einladen und freuen uns auf Ihr Kommen. Ganz besonders bei dieser Jahrestagung freuen wir uns sehr über die erste Teilnahme von Studierenden der Vietnamese German Faculty of Medicine (VGFM, ein Förderprojekt des DVFK), die zurzeit im Klinikum Braunschweig, Wolfsburg, Wolfenbüttel und Herzogin Elisabeth Hospital Braunschweig ihr praktisches Jahr absolvieren. Mit freundlichen Grüßen Prof. Dr. Rolf Engberding Prof. Dr. Si Huyen Nguyen Prof. Dr. Volker Klauss Wolfsburg HCMC/Helmstedt München Diese Fortbildung ist bei der Landesärztekammer Niedersachsen mit 4 CME Punkten anerkannt. PROGRAMM: 8.30 Eröffnung: S.H. Nguyen, Präsident des DVFK / Helmstedt R. Engberding, Präsident GVAC 8:45 Grußwort: M. C. Renneberg, Vize-Präsidentin ÄKN und Vorsitzende der Ärztekammer Bezirksstelle Braunschweig I. Sitzung: Klappenerkrankungen Vorsitz: SH Nguyen (Helmstedt), W. Harringer (Braunschweig) 09:00 Diagnostik und Therapie der Mitralklappeninsuffizienz B. Gerecke (Göttingen) 09:20 Aortenstenose: aktuelle Standards in Diagnostik und Therapie W. Fehske (Köln) 09:40 Chirurgische Therapieoptionen bei Aortenstenose M. Anssar / W. Harringer (Braunschweig) 10:00 Pause II. Sitzung: Interessante Kasuistiken Vorsitz: J. Tebbenjohanns (Hildesheim), W. Fehske (Köln) 10:20 Myokardhypertrophie I. Kruck (Berlin) 10:40 Akuter Myokardinfarkt C. Fleischmann (Wolfsburg) 11:00 Interessante Kasuistik aus Hildesheim J. Tebbenjohanns (Hildesheim) III. Sitzung: Aktuelle Kardiologie im klinischen Alltag Vorsitz: R. Becker (Wolfsburg), W. Diederich (Helmstedt) 11:20 Kardiale Sarkoidose B. Schneider (Lübeck) 11.40 Therapie der chronischen Herzinsuffizienz-Update 2019 B. Gerecke (Göttingen) 12.00 Ablation von Vorhofflimmern: neue Techniken und Strategien D.Q. Nguyen (Köln) 12:20 Diskussionsrunde 12:40 Schlusswort B. Gerecke (Göttingen) Im Anschluss weitere Diskussionen bei einem Imbiss 14:00 DVFK-Mitgliederversammlung REFERENTEN UND GÄSTE:
SPONSOREN DER TAGUNG: Bayer Vital GmbH (1000 €), Daiichi-Sankyo Deutschland GmbH (750 €), Novartis Pharma GmbH (700 €) Stand 60.08.19 22. DVFK-Jahrestagung in BraunschweigHERZLICHE EINLADUNG ZU UNSERER 22. DVFK-JAHRESTAGUNG IN BRAUNSCHWEIG Für Ihre Teilnahme keine Anmeldung erforderlich! Fortbildungsanerkennung: 4 CME Punkte bei Landesärztekammer Niedersachsen! Datum: 01.09.2018 Ort: Ärztehaus, An der Petrikirche 1, 38100 Braunschweig KARDIOMYOPATHIEN Update 2018 & KARDIOLOGIE IM KLINISCHEN ALLTAG PROGRAMM: 8.30 Eröffnung: S.H. Nguyen, Präsident des DVFK / Helmstedt 8:45 Grußwort: D.V. Phuoc, President of the Vietnam Heart Association HCMC I. Sitzung: Kardiomyopathien Update 2018 Vorsitz: J. Tebbenjohanns (Hildesheim) , W. Harringer (Braunschweig) 09:00 Dilatative Kardiomyopathie und Noncompaction Kardiomypathie B. Gerecke (Göttingen) 09:30 Hypertrophe Kardiomyopathie H. Seggewiß (Schweinfurt) 09:50 Arrhythmogene rechtsventrikuläre Kardiomyopathie J. Tebbenjohanns (Hildesheim) 10:10 Chirurgische Therapieoptionen bei Kardiomyopathien M. Anssar / W. Harringer (Braunschweig) 10:30 Pause II. Sitzung: Kardiologie im klinischen Alltag Vorsitz: R. Becker (Wolfsburg) / W. Fehske (Köln) 11.00 Interessante Kasuistik: ein Patient mit Lungenembolie T. Budde (Essen) 11.20 Echokardiographische Beurteilung der Trikuspidalklappe W. Fehske (Köln) 11:40 Moderne Device-Therapie – „State of the Art” S. Winter (Köln) 12:00 Katheterablation bei Vorhofflimmern – aktuelle Studienlage D.Q. Nguyen (Köln) 12:20 Periprozedurale Komplikationen bei der Katheterablation von Vorhofflimmern bei unterschiedlichem Antikoagulationsmanagement H.-F. Vöhringer (Berlin) 12:40 Schlusswort B. Gerecke (Göttingen) Im Anschluss weitere Diskussionen bei einem Imbiss 14:00 DVFK-Mitgliederversammlung REFERENTEN UND GÄSTE:
SPONSOREN DER TAGUNG: Bayer Vital GmbH (1000 €), Biotronik Vertriebs GmbH & Co.KG (500 €), Daiichi-Sankyo Deutschland GmbH (1000 €), Novartis Pharma GmbH (700 €), Medtronic GmbH (300 €) Stand 08/18
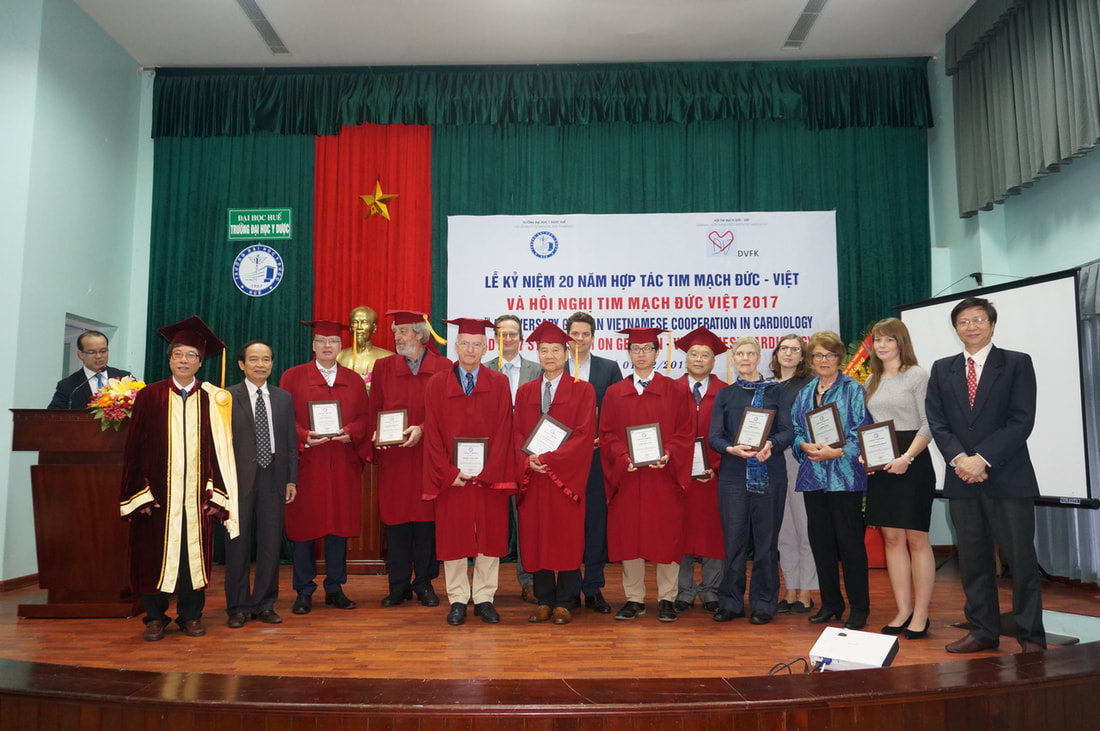
v.l. Dr. Minh (Hue), Prof. Cao Ngoc Thanh (Rektor der Medizinischen Universität Hue), Prof. Tran Huu Dang (Hue), Prof. Volker Klauss (München), Prof. Hans-F. Vöhringer (Berlin), PD Dr. Wolfsgang Fehske (Köln), Prof. Florian Krötz (Starnberg), Prof. Si Huyen Nguyen (HCMC/Helmstedt), Dr. Stefan Winter (Köln), Dr. Dinh Quang Nguyen (Köln), Dr. Tran Thong (USA), Dr. Birke Schneider (Lübeck), Sarah Klauss (München) Dr. Irmtraut Kruck (Ludwigsburg), Dr. Mareike Juliana Brunold (Köln), Prof. Huynh Van Minh (Hue) VIETNAMESE GERMAN SCIENTIFIC SYMPOSIUM HUE 2017 20 Years Anniversary of the German Vietnamese Association of Cardiology (DVFK) 01.12.2017 Venue: Hue University of Medicine and Pharmacy Time: 8:00 – 13:00 Organization: . Hue University of Medicine and Pharmacy . Vietnamese Heart Association Thua Thien Hue . German Vietnamese Association of Cardiology/ Deutsch-Vietnamesischer Förderkreis für Kardiologie e.V. (DVFK) . Vietnamese German Academy for Science and Education in Cardiology and Cardiovascular Surgery (VGAC) Lectures: Echocardiography in oncological diseases Dr. Irmtraut Kruck, Cardiology Clinic, Ludwigsburg, Germany Echocardiography for early detection of cardio toxicity in cancer-patients chemotherapy induces impairment of LV- and RV structure, function and mechanics by different complex mechanism. For this comprehensive assessment of LV/RV structure function and mechanics is necessary in cancer patients before, during and after treatment. Echocardiography is the best image modality because of its availability in every day clinical practice and allows early detection of reduced LV- and RV-function. Therefore it is necessary to perform an echocardiographic examination including all available technics (pulsed and tissue Doppler and 2-D-Strain) in echocardiographic laboratories which have the appropriate equipment and diagnostic expertise. Cardiac dysfunction caused by cardiotoxic treatment can appear at any time during or after therapy and sometimes even after years. Recommendations on the frequency of standardized follow-up examinations exist, but they vary between the specialist societies. Increased morbidity and mortality due to cardiotoxic treatment are now well known, but still too few patients undergo appropriate examinations. Early detection and treatment of existing heart failure and treatment should improve the clinical outcome of these patients. Beyond coronary angiography: Why do we need additional invasive techniques? Prof.Dr. Volker Klauss, Cardiology Munich City Centre, Munich, Germany The decision for interventional treatment of a coronary lesion should be based on symptoms and prove of ischemia. However, in clinical practice, stenoses are often treated depending on the angiographic image, because symptoms are not clear and tests for ischemia have not been performed or the tests are inconclusive. By means of intracoronary pressure measurements (i.e. determination of fractional flow reserve – FFR, or instantaneous wave-free ratio - iFR) the hemodynamic relevance of a coronary stenoses can be determined during coronary angiography especially in intermediate lesions and thus the decision to treat or not to treat is based on an objective test of ischemia. Regarding coronary morphology angiography is the standard for imaging of the coronary tree. However, this technique has limitations. Intravascular ultrasound (IVUS) allows a cross-sectional view of the coronary arteries. IVUS may help to diagnose and assess stent underexpansion and malapposition and to guide interventions in complex cases. Another recent modality based on infrared light is the optical coherence tomography (OCT)with a resolution better than IVUS. It is now used for evaluation of new stent technologies i.e. bioabsorbable scaffolds. Transcatheter treatment of severe mitral regurgitation using the mitraclip system Prof. Dr. Florian Krötz, Clinic Starnberg, Department of Cardiology, 82319 Starnberg, Germany The interventional treatment of mitral valve regurgitation using the MitraClip procedure is a valuable tool for treatment of inoperable patients or patients at high operative risk. Its efficiency in reducing mitral regurgitation has been proven in the EVEREST II study, and use of the technique has rapidly grown worldwide and especially in Germany since then. In suitable patients the method is excellent for treating primary mitral valve regurgitation but has also great potential in patients with heart failure and secondary mitral valve regurgitation, which often show poor outcomes following surgery. Current recommendations and clinical data concerning the method rely largely on data from the EVEREST II trial. Registries, like the German TRAMI register however, survey a large number of patients, so today there is a good insight into the prerequisites of building an interventional mitral valve program, the need for specialized screening of patients, and for a dedicated interventional setup during implantation. This and the essential procedural techniques will be outlined. Catheter Ablation of Atrial Fibrillation in Patients with heart Failure: Evidence for prognostic indication? Dr. Dinh Quang Nguyen, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Catheter Ablation of Atrial fibrillation is well established in symptomatic patients. But it is still a symptomatic indication. In Patients with reduced LV ejection fraction and heart failure, the success rate of catheter ablation remains challenging and controversial. This presentation gives an update in publications and highlights a new published randomized study (Castle-AF), which has shown a prognostic benefit of catheter ablation in Patients with heart failure. Diagnostic value of cardiac MRI in patients with heart failure Dr. Birke Schneider, Lübeck, Germany Heart Failure (HF) is a clinical syndrome characterized by typical symptoms and clinical signs which are caused by a structural and/ or functional cardiac abnormality, resulting in reduced cardiac output and/ or elevated intracardiac pressures at rest or during stress. Demonstration of an underlying cardiac cause is central to the diagnosis of HF. This is usually a myocardial abnormality causing systolic and/or diastolic ventricular dysfunction. However, abnormalities of the valves, pericardium, endocardium, heart rhythm and conduction can also cause HF, and more than one abnormality is often present. Identification of the underlying cardiac problem is crucial for therapeutic reasons, as the precise pathology determines the specific treatment used. Cardiac imaging plays a central role in the diagnosis of HF and in guiding treatment. Of several imaging modalities available, echocardiography is the method of choice in patients with suspected HF, for reasons of accuracy, availability (including portability), safety and cost. However, the reliability of the echocardiographic study is highly dependent on the operator and centre experience and the image quality. Transthoracic echocardiography (TTE) nevertheless is regarded the primary method for assessment of systolic and diastolic function of both left and right ventricles and for the evaluation of valvular function. Cardiac magnetic resonance imaging (CMRI) is nowadays acknowledged as the gold standard for the measurements of volumes, mass and ejection fraction of both the left and right ventricles (Class I Level C in the ESC Guidelines on HF 2016). It is the best alternative cardiac imaging modality for patients with nondiagnostic echocardiographic studies (particularly for imaging of the right heart) and is the method of choice in patients with complex congenital heart diseases. In addition, CMRI also allows tissue characterization and thereby can be useful for establishing HF aetiology. CMRI is the preferred imaging method to assess myocardial fibrosis using late gadolinium enhancement (LGE) along with T1 mapping. CMRI with LGE allows differentiation between ischaemic and non-ischaemic origins of HF and myocardial fibrosis/ scars can be visualized. Different hyperenhancement patterns result from the pathophysiology of the underlying disease and help to establish the correct diagnosis. CMRI may also be used for the assessment of myocardial ischaemia and viability in patients with HF and coronary artery disease. Various patients are presented where CMRI was essential in finding the cause of HF and had implications for patient management. Clinical limitations of CMRI will also be discussed. Risk of major adverse cardiac events following noncardiac surgery in patients with coronary stents Prof. Dr. Hans-F. Voehringer, DRK Clinics Berlin, Germany Surgeons, cardiologists, primary care physicians, and anesthesiologists frequently have to determine the antiplatelet management in patients with coronary heart disease undergoing elective surgery. In Germany, more than 300 000 patients receive coronary stents annually, with up to 20% of these individuals requiring non-cardiac surgery within 2 years. There is definitive evidence that patients who have undergone percutaneous coronary interventions with stent implantation are at increased risk of perioperative major cardiac events (MACE) and that the risk is moderated by stent type (bare metal stent [BMS] vs. drug eluting stent [DES]), operative urgency, early discontinuation of antiplatelet therapy, and time from coronary intervention. Guidelines recommend delaying non-cardiac surgery in patients after coronary stent procedure for 1 year after DES and for 6 weeks after BMS. The evidence underlying these recommendations is limited and conflicting. In a systematic review the perioperative antiplatelet management will be assessed to help clinicians with this common clinical case. 3D Echocardiography, from research to routine application: Today an obligatory application for a comprehensive investigation of the heart PD Dr. Wolfgang Fehske, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany A comprehensive investigation of systolic and diastolic heart failure patients by echocardiography PD Dr. Wolfgang Fehske, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Left atrial function, what can we derive from echocardiographic examinations with special respect to prognosis of stability after electrophysiological ablation for atrial fibrillation Mareike Juliana Brunold, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Real world experience with resynchronization therapy: A detailed overview of more than 400 consecutive patients treated according to the guidelines Stefan Winter, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Sudden cardiac death beyond the existing guidelines: Does the Life Vest concept opens better solutions for our patients? Stefan Winter, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany FACULTY: Dr. Mareike Juliana Brunold, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany PD Dr. Wolfgang Fehske, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Prof. Dr. Volker Klauss, Cardiology Munich City Centre, Munich, Germany Prof. Dr. Florian Krötz, Clinic Starnberg, Department of Cardiology, 82319 Starnberg, Germany Dr. Irmtraut Kruck, Cardiology Clinic Ludwigsburg, Germany Dr. Dinh Quang Nguyen, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Prof. Dr. Si Huyen Nguyen, Vietnamese German Faculty of Medicine at Pham Ngoc Thach University HCMC, HELIOS St. Marienberg Hospital Helmstedt, Germany Dr. Birke Schneider, MD, Lübeck, Germany Prof. Dr. Hans-F. Voehringer, DRK Clinics Berlin, Germany Dr. Stefan Winter, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Ehrenplakette für Prof. Si Huyen Nguyen (HCMC/Helmstedt) und Prof. Volker Klauss (München), überreicht vom Herrn Nguyen Van Phuong, stellvertretenden Gouverneur von Thua Thien-Hue  Prof. F. Krötz (Starnberg) Prof. V. Klauss (München) bei der HKU mit dem Ärzteteam der Universität Hue Gruppenbild mit Prof. V. Klauss. An der rechten Seite von Prof. Klauss ist Prof. H.A. Tien, Leiter des HKLs der Universitätsklinik Hue.
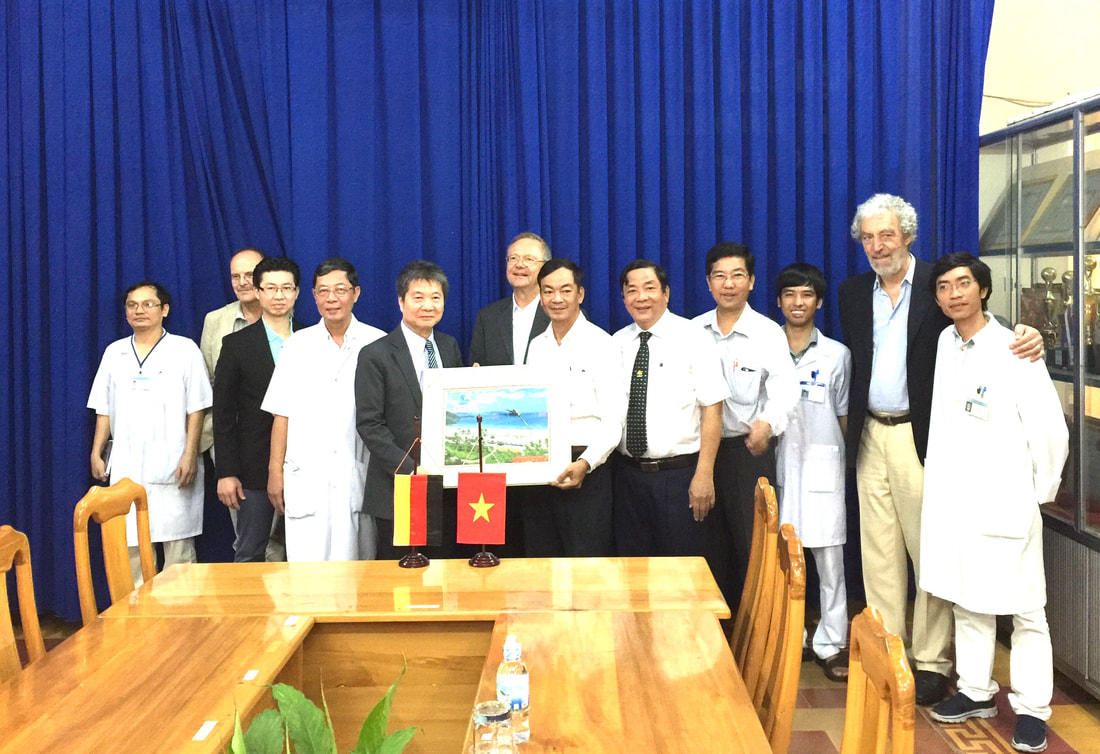
VIETNAMESE GERMAN SCIENTIFIC SYMPOSIUM 2017 Nha Trang/Khanh Hoa 28.11.2017 20 Years Anniversary of the German Vietnamese Association of Cardiology (DVFK) Venue: KHANH HOA HOSPITAL Time: 13:30 – 17:00 Organization: . Vietnamese Heart Association Khanh Hoa . Khanh Hoa Hospital . German Vietnamese Association of Cardiology/ Deutsch-Vietnamesischer Förderkreis für Kardiologie e.V. (DVFK) . Vietnamese German Academy for Science and Education in Cardiology and Cardiovascular Surgery (VGAC) . Vietnamese German Faculty of Medicine of Pham Ngoc Thach University of Medicine at Ho Chi Minh City (VGFM) Lectures: Echocardiography in oncological diseases Dr. Irmtraut Kruck, Cardiology Clinic, Ludwigsburg, Germany Echocardiography for early detection of cardio toxicity in cancer-patients chemotherapy induces impairment of LV- and RV structure, function and mechanics by different complex mechanism. For this comprehensive assessment of LV/RV structure function and mechanics is necessary in cancer patients before, during and after treatment. Echocardiography is the best image modality because of its availability in every day clinical practice and allows early detection of reduced LV- and RV-function. Therefore it is necessary to perform an echocardiographic examination including all available technics (pulsed and tissue Doppler and 2-D-Strain) in echocardiographic laboratories which have the appropriate equipment and diagnostic expertise. Cardiac dysfunction caused by cardiotoxic treatment can appear at any time during or after therapy and sometimes even after years. Recommendations on the frequency of standardized follow-up examinations exist, but they vary between the specialist societies. Increased morbidity and mortality due to cardiotoxic treatment are now well known, but still too few patients undergo appropriate examinations. Early detection and treatment of existing heart failure and treatment should improve the clinical outcome of these patients. Beyond coronary angiography: Why do we need additional invasive techniques? Prof.Dr. Volker Klauss, Cardiology Munich City Centre, Munich, Germany The decision for interventional treatment of a coronary lesion should be based on symptoms and prove of ischemia. However, in clinical practice, stenoses are often treated depending on the angiographic image, because symptoms are not clear and tests for ischemia have not been performed or the tests are inconclusive. By means of intracoronary pressure measurements (i.e. determination of fractional flow reserve – FFR, or instantaneous wave-free ratio - iFR) the hemodynamic relevance of a coronary stenoses can be determined during coronary angiography especially in intermediate lesions and thus the decision to treat or not to treat is based on an objective test of ischemia. Regarding coronary morphology angiography is the standard for imaging of the coronary tree. However, this technique has limitations. Intravascular ultrasound (IVUS) allows a cross-sectional view of the coronary arteries. IVUS may help to diagnose and assess stent underexpansion and malapposition and to guide interventions in complex cases. Another recent modality based on infrared light is the optical coherence tomography (OCT)with a resolution better than IVUS. It is now used for evaluation of new stent technologies i.e. bioabsorbable scaffolds. Transcatheter treatment of severe mitral regurgitation using the mitraclip system Prof. Dr. Florian Krötz, Clinic Starnberg, Department of Cardiology, 82319 Starnberg, Germany The interventional treatment of mitral valve regurgitation using the MitraClip procedure is a valuable tool for treatment of inoperable patients or patients at high operative risk. Its efficiency in reducing mitral regurgitation has been proven in the EVEREST II study, and use of the technique has rapidly grown worldwide and especially in Germany since then. In suitable patients the method is excellent for treating primary mitral valve regurgitation but has also great potential in patients with heart failure and secondary mitral valve regurgitation, which often show poor outcomes following surgery. Current recommendations and clinical data concerning the method rely largely on data from the EVEREST II trial. Registries, like the German TRAMI register however, survey a large number of patients, so today there is a good insight into the prerequisites of building an interventional mitral valve program, the need for specialized screening of patients, and for a dedicated interventional setup during implantation. This and the essential procedural techniques will be outlined. Catheter Ablation of Atrial Fibrillation in Patients with heart Failure: Evidence for prognostic indication? Dr. Dinh Quang Nguyen, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Catheter Ablation of Atrial fibrillation is well established in symptomatic patients. But it is still a symptomatic indication. In Patients with reduced LV ejection fraction and heart failure, the success rate of catheter ablation remains challenging and controversial. This presentation gives an update in publications and highlights a new published randomized study (Castle-AF), which has shown a prognostic benefit of catheter ablation in Patients with heart failure. Diagnosis and Management of patients with inherited primary arrhythmia syndromes Risk stratification in a family with Long QT-Syndrome Dr. Birgit Gerecke, outpatient center cardiology Peine When the diagnosis of an inherited primary arrhythmia syndrome is made, considerations on the management also of other family members are required. This is shown exemplary in a family with LQTS. A 16 year old girl presented with recurrent syncope. The examinations of the family doctor contained an ECG. A prolongation of the QT interval was seen without a secondary cause of QT prolongation. The patient was admitted to a hospital. ECG monitoring showed runs of torsades de pointes VT. Beta blocker therapy was initiated, but still runs of VT were present. The diagnosis of a LQTS 2 was established. Family history revealed a sudden cardiac death in a great uncle of the index patient. ICD implantation was discussed and after informed consenta single chamber ICD system was implanted. Till now there has been no adequate shock delivery in the patient. ECGs of the parents and two siblings were done. The mother also presented with a QT prolongation, but till now is asymptomatic. A younger sister has a borderline QTc, the ECG of the brother showed a normal QTc. Genetic testing was done in the family with the presence of an LQTS gene mutation (KCNH2mutation) in the index patient. This mutation was also found in her mother, but not in the siblings. LQT-Syndrom is an inherited arrhythmia syndrome with a broad spectrum of clinical presentations, even in one family. A family based genetic testing can help to stratify the management. An exclusion of an assured mutation of the index patient in other family members can rule out the risk of a rhythmogenic disease and event with a high probability. Life style changes are recommended for family members with the mutation containing the avoidance of QT prolonging drugs, the identification and correction of electrolyte abnormalities, beta-blockers or ICD-implantation depending on the clinical presentation. Approximately 20-25 % of patients with LQTS confirmed by the presence of an LQTS gene mutation may have a normal QTc. Provocative tests with QT measurement e.g. in the recovery phase of exercise testing can help to unmask these patients. Diagnostic value of cardiac MRI in patients with heart failure Dr. Birke Schneider, Lübeck, Germany Heart Failure (HF) is a clinical syndrome characterized by typical symptoms and clinical signs which are caused by a structural and/ or functional cardiac abnormality, resulting in reduced cardiac output and/ or elevated intracardiac pressures at rest or during stress. Demonstration of an underlying cardiac cause is central to the diagnosis of HF. This is usually a myocardial abnormality causing systolic and/or diastolic ventricular dysfunction. However, abnormalities of the valves, pericardium, endocardium, heart rhythm and conduction can also cause HF, and more than one abnormality is often present. Identification of the underlying cardiac problem is crucial for therapeutic reasons, as the precise pathology determines the specific treatment used. Cardiac imaging plays a central role in the diagnosis of HF and in guiding treatment. Of several imaging modalities available, echocardiography is the method of choice in patients with suspected HF, for reasons of accuracy, availability (including portability), safety and cost. However, the reliability of the echocardiographic study is highly dependent on the operator and centre experience and the image quality. Transthoracic echocardiography (TTE) nevertheless is regarded the primary method for assessment of systolic and diastolic function of both left and right ventricles and for the evaluation of valvular function. Cardiac magnetic resonance imaging (CMRI) is nowadays acknowledged as the gold standard for the measurements of volumes, mass and ejection fraction of both the left and right ventricles (Class I Level C in the ESC Guidelines on HF 2016). It is the best alternative cardiac imaging modality for patients with nondiagnostic echocardiographic studies (particularly for imaging of the right heart) and is the method of choice in patients with complex congenital heart diseases. In addition, CMRI also allows tissue characterization and thereby can be useful for establishing HF aetiology. CMRI is the preferred imaging method to assess myocardial fibrosis using late gadolinium enhancement (LGE) along with T1 mapping. CMRI with LGE allows differentiation between ischaemic and non-ischaemic origins of HF and myocardial fibrosis/ scars can be visualized. Different hyperenhancement patterns result from the pathophysiology of the underlying disease and help to establish the correct diagnosis. CMRI may also be used for the assessment of myocardial ischaemia and viability in patients with HF and coronary artery disease. Various patients are presented where CMRI was essential in finding the cause of HF and had implications for patient management. Clinical limitations of CMRI will also be discussed. Risk of major adverse cardiac events following noncardiac surgery in patients with coronary stents Prof. Dr. Hans-F. Voehringer, DRK Clinics Berlin, Germany Surgeons, cardiologists, primary care physicians, and anesthesiologists frequently have to determine the antiplatelet management in patients with coronary heart disease undergoing elective surgery. In Germany, more than 300 000 patients receive coronary stents annually, with up to 20% of these individuals requiring non-cardiac surgery within 2 years. There is definitive evidence that patients who have undergone percutaneous coronary interventions with stent implantation are at increased risk of perioperative major cardiac events (MACE) and that the risk is moderated by stent type (bare metal stent [BMS] vs. drug eluting stent [DES]), operative urgency, early discontinuation of antiplatelet therapy, and time from coronary intervention. Guidelines recommend delaying non-cardiac surgery in patients after coronary stent procedure for 1 year after DES and for 6 weeks after BMS. The evidence underlying these recommendations is limited and conflicting. In a systematic review the perioperative antiplatelet management will be assessed to help clinicians with this common clinical case. A comprehensive investigation of systolic and diastolic heart failure patients by echocardiography PD Dr. Wolfgang Fehske, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Left atrial function, what can we derive from echocardiographic examinations with special respect to prognosis of stability after electrophysiological ablation for atrial fibrillation Mareike Juliana Brunold, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Sudden cardiac death beyond the existing guidelines: Does the Life Vest concept opens better solutions for our patients? Stefan Winter, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany FACULTY: Dr. Mareike Juliana Brunold, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany PD Dr. Wolfgang Fehske, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Dr. Birgit Gerecke, outpatient center cardiology Peine, Germany Prof. Dr. Volker Klauss, Cardiology Munich City Centre, Munich, Germany Prof. Dr. Florian Krötz, Clinic Starnberg, Department of Cardiology, 82319 Starnberg, Germany Dr. Irmtraut Kruck, Cardiology Clinic Ludwigsburg, Germany Dr. Dinh Quang Nguyen, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Prof. Dr. Si Huyen Nguyen, Vietnamese German Faculty of Medicine at Pham Ngoc Thach University HCMC, HELIOS St. Marienberg Hospital Helmstedt, Germany Dr. Birke Schneider, MD, Lübeck, Germany Prof. Dr. Hans-F. Voehringer, DRK Clinics Berlin, Germany Stefan Winter, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Visite auf einer Station der kardiologischen Abteilung v.l. S. Klauss (München), Dr. I. Kruck (Ludwigsburg), Dr. B. Gerecke (Peine), Dr. M.J. Brunold (Köln), Dr. B. Schneider (Lübeck)
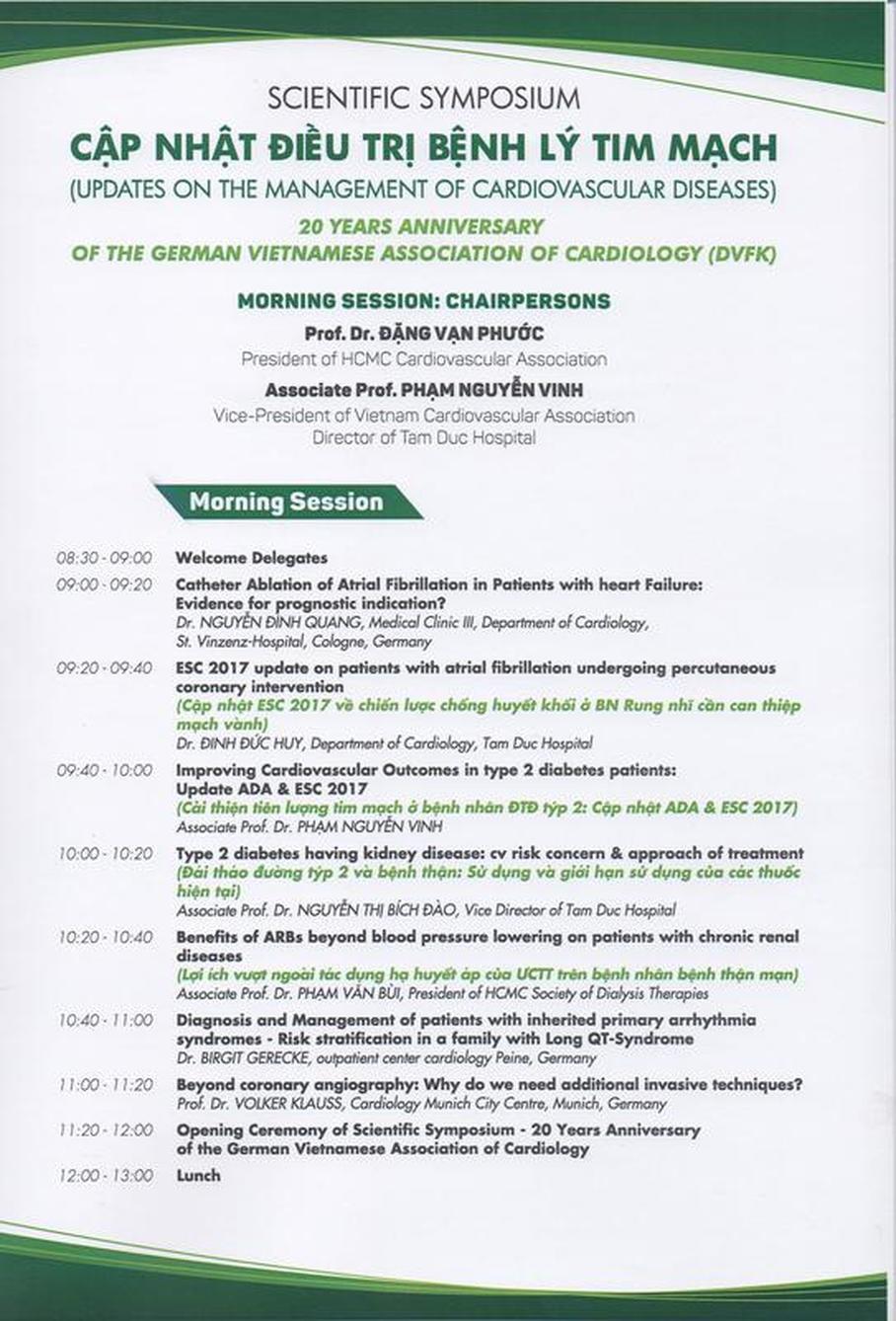
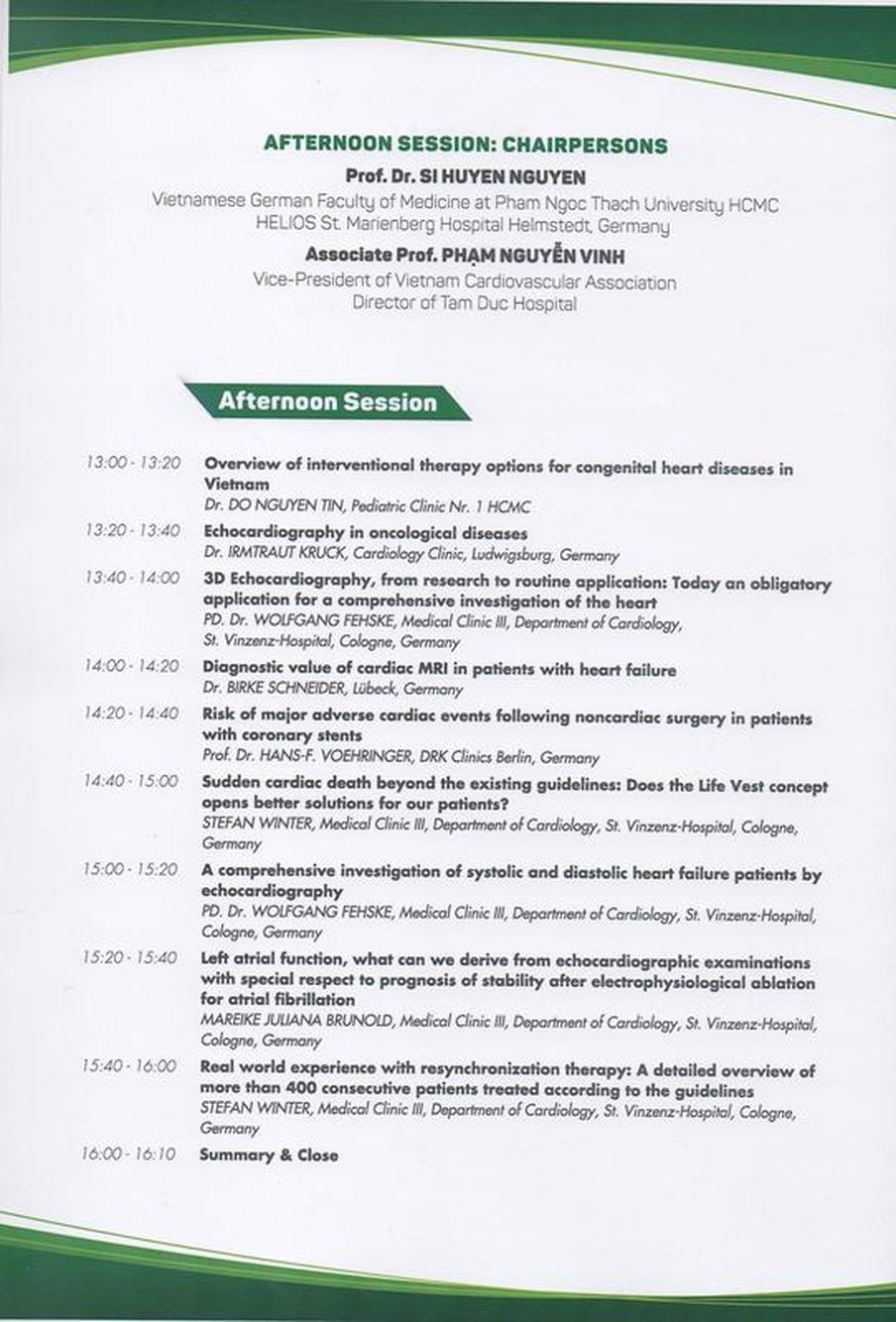
17. VIETNAMESE GERMAN HEART DAYS HCMC 26.11.2017 Venue: NEW WORLD HOTEL, 76 Le Lai Street, District 1, HCMC Time: 08:30 - 16:30 Organization: HCMC Cardiovascular Association in Cooperation with
 v.l. Dr. B. Schneider (Lübeck), S. Klauss (München), Dr. B. Gerecke (Peine), Prof. PV Bui (HCMC), Prof. H.-F. Vöhringer (Berlin), Prof. V. Klauss (München), Prof. NT Binh (HCMC), Prof. SH Nguyen (HCMC/Helmstedt), Dr. G. Haug (Bayerisch Gmain), Prof. DV Phuoc (HCMC), Prof. PN Vinh (HCMC), Dr. S. Winter (Köln), PD Dr. W. Fehske (Köln), Dr. I. Kruck (Ludwigsburg), Dr. DQ Nguyen (Köln), Dr. MJ Brunold (Köln) Echokardiographie bei onkologischen Erkrankungen (Dr. Irmtraut Kruck/Ludwigsburg) 21. DVFK-JAHRESTAGUNG IN BRAUNSCHWEIG Datum: 02.09.2017 Ort: Ärztehaus, An der Petrikirche 1, 38100 Braunschweig AKTUELLE KARDIOLOGIE & INTERESSANTE KASUISTIKEN PROGRAMM: 8.30 Eröffnung: S.H. Nguyen, Präsident DVFK / Helmstedt 8.40 Begrüßung: M. C. Renneberg, Vizepräsidentin der Ärztekammer Niedersachsen (ÄKN) und Vorsitzende der ÄKN Bezirksstelle Braunschweig D.V. Phuoc, President of Vietnam Heart Association HCMC 8.55 Einleitung: R. Engberding, Präsident VGAC/Wolfsburg I. Sitzung: Kardiologie in Kooperationen Vorsitz: R. Engberding (Wolfsburg), W. Harringer (Braunschweig) 09:00 Echokardiographie bei onkologischen Erkrankungen I.Kruck (Ludwigsburg) 09:20 Interdisziplinäres Konzept bei TAVI und Aortenchirurgie im Hybrid-OP Chronische Herzinsuffizienz: eine interdisziplinäre Herausforderung W. Harringer / M. Anssar (Braunschweig) 09:40 Akuttherapie des ischämischen Schlaganfalls L. Harms (Berlin) II.Sitzung: Diagnostik in der Kardiologie Vorsitz: B. Gerecke (Peine) / W. Fehske (Köln) 10:00 Kardiale MRT-Diagnostik bei Herzinsuffizienz B. Schneider (Lübeck) 10:20 „Der wahre und der falsche Mobitz - warum in Deutschland so viele Herzschrittmacher implantiert werden“ K. von Olshausen (Heidelberg) 10:40 Gendiagnostik bei kardiovaskulären Erkrankungen: Stand 2017 B. Gerecke (Peine) 11:00 Pause III.Sitzung: Interessante Kasuistiken Vorsitz: GD Kneissl (Mainz) / W-K. Diederich (Helmstedt) 11.30 Patient mit ventrikulärer Tachykardie L. Lichtenberg (Köln) 11:50 Vorhofflimmern und Herzinsuffizienz D. Q. Nguyen (Köln) 12:10 Pat. mit chronischem Koronarverschluss C. Fleischmann (Wolfsburg) 12:30 Schlusswort B. Gerecke (Peine) Im Anschluss weitere Diskussionen bei einem Imbiss 14:00 DVFK-Mitgliederversammlung REFERENTEN UND GÄSTE:
SPONSOREN DER TAGUNG: Bayer Vital GmbH (1000 €), Biotronik Vertriebs GmbH & Co.KG (500 €), Boehringer Ingelheim Pharma GmbH & Co.KG (500 €), Daiichi-Sankyo Deutschland GmbH (750 €), Medtronic GmbH (300 €), Novartis Pharma GmbH (700 €), SERVIER Deutschland GmbH (500 €) Grußwort von Prof. Dang Van Phuoc, Präsident der kardiologischen Gesellschaft der Ho-Chi-Minh-Stadt Kardiale MRT-Diagnostik bei Herzinsuffizienz /Birke Schneider (Lübeck) Patient mit ventrikulärer Tachykardie / Dr. Lutz Lichtenberg (Köln)
VIETNAMESE GERMAN SCIENTIFIC SYMPOSIUM HUE
01.12.2016 Venue: Hue University of Medicine and Pharmacy Hue University Hospital Times: 8:00 - 13:00 Organization: Hue University of Medicine and Pharmacy in Cooperation with
Lectures: Atrial Fibrillation - Update 2016: New Guidelines, Ablative Treatment, Drugs, Studies Dr. Dinh Quang Nguyen, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Ventricular Tachycardia - Update 2016: Guidelines, Ablative Treatment, Drugs, Studies Dr. Dinh Quang Nguyen, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Antitcoagulation and Antithrombotic Therapy in Patients with Atrial Fibrillation (AF) and Acute Coronary Syndrome – Update 2016 Prof. Dr. Hans-F. Voehringer, Clinical Research Centre, DRK Kliniken I Koepenick, Germany Transradial vs. transfemoral access in patients with ACS: Bleeding complications and Outcome Dr. Ralph Schoeller (on behalf of Berlin Myocardial Infarction Registry), Clinic for Cardiology of DRK Kliniken Berlin I Westend, Germany Cardiac Rehabilitation – Update 2016 Günter Haug, M.D., FESC , Rehabilitation Center, German Pension Insurance Federation, Bayerisch Gmain, Germany Non-invasive positive pressure ventilation for the treatment of chronic obstructive pulmonary disease (COPD) - Update 2016 Prof. Dr. Si Huyen Nguyen, Vietnamese German Faculty of Medicine at Pham Ngoc Thach University of Medicine HCMC, HELIOS St. Marienberg Hospital Helmstedt, Academic Hospital of the Otto-von-Guericke University Magdeburg, Germany FACULTY: Günter Haug, M.D., FESC , Rehabilitation Center, German Pension Insurance Federation, Bayerisch Gmain, Germany Dr. Dinh Quang Nguyen, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Köln, Germany Prof. Dr. Si Huyen Nguyen, Vietnamese German Faculty of Medicine at Pham Ngoc Thach University of Medicine HCMC, HELIOS St. Marienberg Hospital Helmstedt, Academic Hospital of the Otto-von-Guericke University Magdeburg, Germany Dr. Ralph Schoeller, Clinic for Cardiology of DRK Kliniken Berlin I Westend, Germany Prof. Dr. Hans-F. Voehringer, Clinical Research Centre, DRK Kliniken I Koepenick, Germany 6. VIETNAMESE GERMAN SCIENTIFIC SYMPOSIUM NHA TRANG
29.11.2016 Venue: General Hospital Khanh Hoa Times: 14:00 -17:00 Organization: General Hospital Khanh Hoa in Cooperation with
Lectures: Atrial Fibrillation - Update 2016: New Guidelines, Ablative Treatment, Drugs, Studies Dr. Dinh Quang Nguyen, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Ventricular Tachycardia - Update 2016: Guidelines, Ablative Treatment, Drugs, Studies Dr. Dinh Quang Nguyen, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Antitcoagulation and Antithrombotic Therapy in Patients with Atrial Fibrillation (AF) and Acute Coronary Syndrome – Update 2016 Prof. Dr. Hans-F. Voehringer, Clinical Research Centre, DRK Kliniken I Koepenick, Germany Transradial vs. transfemoral access in patients with ACS: Bleeding complications and Outcome Dr. Ralph Schoeller (on behalf of Berlin Myocardial Infarction Registry), Clinic for Cardiology of DRK Kliniken Berlin I Westend, Germany Cardiac Rehabilitation – Update 2016 Günter Haug, M.D., FESC , Rehabilitation Center, German Pension Insurance Federation, Bayerisch Gmain, Germany Non-invasive positive pressure ventilation for the treatment of chronic obstructive pulmonary disease (COPD) - Update 2016 Prof. Dr. Si Huyen Nguyen, Vietnamese German Faculty of Medicine at Pham Ngoc Thach University of Medicine HCMC, HELIOS St. Marienberg Hospital Helmstedt, Academic Hospital of the Otto-von-Guericke University Magdeburg, Germany FACULTY: Dr. Günter Haug, FESC , Rehabilitation Center, German Pension Insurance Federation, Bayerisch Gmain, Germany Dr. Dinh Quang Nguyen, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Köln, Germany Prof. Dr. Si Huyen Nguyen, Vietnamese German Faculty of Medicine at Pham Ngoc Thach University of Medicine HCMC, HELIOS St. Marienberg Hospital Helmstedt, Academic Hospital of the Otto-von-Guericke University Magdeburg, Germany Dr. Ralph Schoeller, Clinic for Cardiology of DRK Kliniken Berlin I Westend, Germany Prof. Dr. Hans-F. Voehringer, Clinical Research Centre, DRK Kliniken I Koepenick, Germany 16. VIETNAMESE GERMAN HEART DAYS 2016
SCIENTIFIC SYMPOSIUM HCMC 27.11.2016 Organization: Vietnamese Heart Association of Ho Chi Minh City in Cooperation with
Lectures: Atrial Fibrillation - Update 2016: New Guidelines, Ablative Treatment, Drugs, Studies Dr. Dinh Quang Nguyen, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Summary:
Ventricular Tachycardia - Update 2016: Guidelines, Ablative Treatment, Drugs, Studies Dr. Dinh Quang Nguyen, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Cologne, Germany Summary:
Antitcoagulation and Antithrombotic Therapy in Patients with Atrial Fibrillation (AF) and Acute Coronary Syndrome – Update 2016 Prof. Dr. Hans-F. Voehringer, Clinical Research Centre, DRK Kliniken I Koepenick, Germany Background: Guidelines for treatment of atrial fibrillation (AF) and coronary revascularisation recommend individual treatment regimen for patients with AF and acute coronary syndrome (ACS) according to their risk of bleeding or suffering from thrombo-embolic complications. The aim of the present study is to illustrate how guidelines are implemented into daily practice and whether treatment approaches have changed over time since the introduction of new oral anticoagulants (NOACs). Methods and Results: From January 2011 to December 2014 we included 1537 AF patients with ACS into a registry (Berlin Myocardial Infarction Registry) collecting data on hospital treatment, hospital mortality, and discharge medication. 790 out of these patients received DES (51.4%), 277 BMS (18%), 125 only balloon dilatation (8.1%) and 345 no intervention (22.4%), respectively. 95 % of patients had a CHA2DS2-VASc Score >1, the hospital mortality amounted to 9.8%. Table 1: Anticoagulation for AF patients with ACS discharged from hospital with CHA2DS2-VASc Score >1 Table 2: Discharge medication for patients treated with stents dismissed from hospital with CHA2DS2-VASc Score >1 Conclusion: In Tab 1 and 2 the percentage of patients treated with anticoagulation is seen over a time period of 4 years. While the percentage of patients treated with heparin and Vitamin-K antagonists has remained the same, those patients treated with NOACs have increased. Nearly 60% of AF patients with ACS received a triple therapy. The findings will be discussed in light of published data in the literature. Newer and specifically designed trials are awaited for further improvement of the existing knowledge about efficacy and safety of this combination therapy. Transradial vs. transfemoral access in patients with ACS: Bleeding complications and Outcome Dr. Ralph Schoeller (on behalf of Berlin Myocardial Infarction Registry), Clinic for Cardiology of DRK Kliniken Berlin I Westend, Germany Background: The use of transradial access for PCI is growing and the newly published guidelines on treatment of ACS take account of this, provided the necessary experience exists. We studied ways of access in treatment of ACS patients under real world conditions in a big city. Methods: Our Registry collects data on hospital treatment of patients with ACS since 1999. Since 1.4.2011 data on different ways of PCI access are collected. In our study we included all 10,146 patients treated with PCI from 20 hospitals between 1.4.11-31.12.14. We studied bleeding complications according to GUSTO criteria (mild, moderate, severe) and we analysed the influence of transfemoral vs. transradial access on hospital mortality. Results: 4165 patients were treated with transradial (41,1%), 5981 with transfemoral (58,9%) PCI access. Transfemoral vs. transradial access influences hospital mortality (OR=1.53; 95% CI: 1.18–1.98) and also influences chances of moderate to severe bleeding (OR=1.69; 95% CI: 1.17–2.45) even after adjustment for differences in patient characteristics and in antiplatelet and antithrombotic therapy. Table: Differences between patients with transradial vs. transfemoral access Conclusion:
Cardiac Rehabilitation – Update 2016 Günter Haug, M.D., FESC , Rehabilitation Center, German Pension Insurance Federation, Bayerisch Gmain, Germany The aim of this lecture is to give an update 2016 of cardiac rehabilitation (rehab) according to international guidelines (AHA, AAVPR, EAPR of ESC) focussed on strategies how to organize modern cardiac rehab. Class I indications for post-surgical and post-interventional referral and logistic feasibilities to transfer these eligible patients to in-patient resident or out-patient cardiac rehab units will be presented. Evidence based benefits and safety as well as concerns and risks of early and continued cardiac rehab are described. Based on our experience out of a 230-bed cardiac rehabilitation center overlooking more than 3000 in-patient rehab cases a year we discuss requirements for structures, core competencies of staff and core components of cardiac rehab in the different phases of recovery. Guideline based programs covering the 5 core components of cardiac rehab, in particular supervised exercise training, patient education on specific heart condition of cardiovascular diseases (CVD) as well as strategies to improve risk factors and to stop smoking, to achieve medication adherence and emotional recovery will be presented. We therefore demonstrate in particular rehab specific medical admission, rehabilitation care, risk stratification, prescription of supervised exercise training, courses to improve risk factors considering country specific needs as well as to achieve medication adherence. The objectives of early and continued cardiac rehab are to overcome postoperative and post-interventional physical and functional handicaps, to avoid early complications, further cardiac events and progression of CVD, to cope with psychosocial problems, and to reintegrate in job and family. In summery core components of modern cardiac rehabilitation will be presented based on our specific experience and according to latest study results and current guidelines. Roadmaps how to organize cardiac rehab in order to improve early and long-term outcome and last but not least in order to discharge acute hospital wards, to raise the number of operations and interventions, and therefore to increase the number of treatable patients esp. in low-resource settings will be discussed. Non-invasive positive pressure ventilation for the treatment of chronic obstructive pulmonary disease (COPD) - Update 2016 Prof. Dr. Si Huyen Nguyen, Vietnamese German Faculty of Medicine at Pham Ngoc Thach University of Medicine HCMC, HELIOS St. Marienberg Hospital Helmstedt, Academic Hospital of the Otto-von-Guericke University Magdeburg, Germany The non-invasive ventilation (NIV) has been established for about 20 years as a successful treatment method for acute respiratory insufficiency (ARI), as home ventilation it has been used in the last 10 years by hypercapnic COPD patients increasingly. A persistent hypercapnia for medically treated patients with COPD is a manifest sign of the failure of the respiratory pump and thus indicates a poor prognosis of the disease. It is also regarded as a criterion for initiating nocturnal home ventilation with a non-invasive, pressure-controlled ventilation (NPPV). This measure is primarily to improve the quality of life. In a recently published study by Köhnlein et al a relevant life extension by NPPV has now been documented in patients with a chronic failure of the respiratory pump in COPD for the first time. The pathophysiology of COPD, indications and contraindications for NIV in ARI and nocturnal home ventilation, techniques and practical application of non-invasive ventilation are presented. FACULTY: Dr. Günter Haug, FESC , Rehabilitation Center, German Pension Insurance Federation, Bayerisch Gmain, Germany Dr. Dinh Quang Nguyen, Medical Clinic III, Department of Cardiology, St. Vinzenz-Hospital, Köln, Germany Prof. Dr. Si Huyen Nguyen, Vietnamese German Faculty of Medicine at Pham Ngoc Thach University of Medicine HCMC, HELIOS St. Marienberg Hospital Helmstedt, Academic Hospital of the Otto-von-Guericke University Magdeburg, Germany Dr. Ralph Schoeller, Clinic for Cardiology of DRK Kliniken Berlin I Westend, Germany Prof. Dr. Hans-F. Voehringer, Clinical Research Centre, DRK Kliniken I Koepenick, Germany |
Archiv
November 2019
|
|||||||||||||||








































 RSS Feed
RSS Feed
